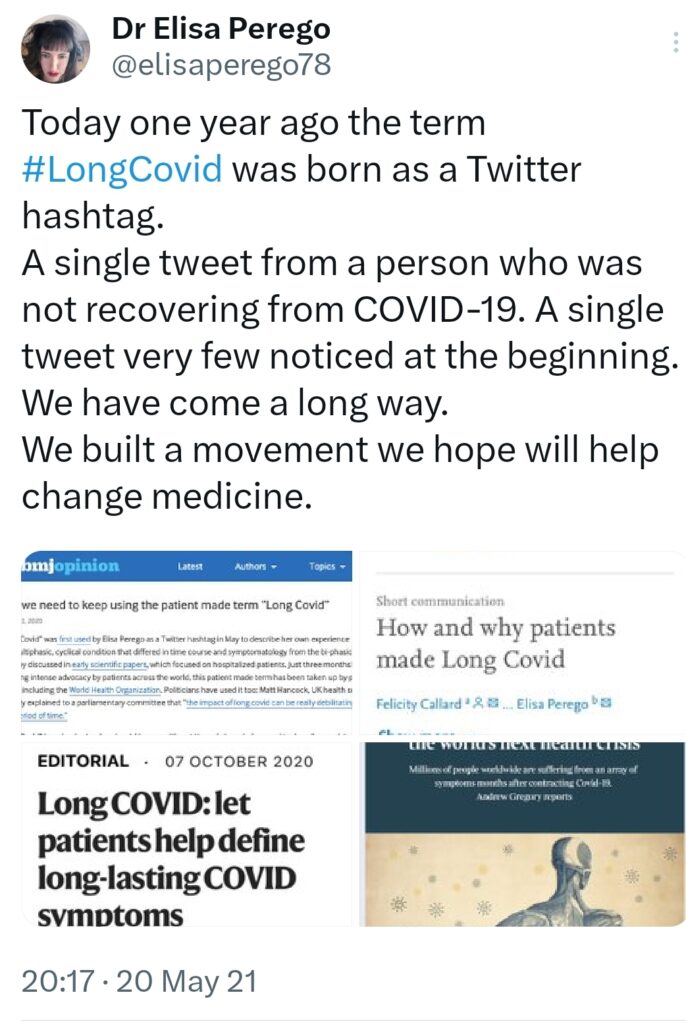
76- 01/06/2024 In 2020, Elisa Perego, a Ph.D. in archaeology, was living in Lombardy (Italy) where she contracted the SARS-CoV-2 and witnessed with horror its rapid spread. During the lockdown and despite her severe health problems, she exchanged with other patients via Twitter/X. She then observed with her peers that COVID-19 could last much longer than the two to six weeks indicated in the initial reports and that the symptoms were not solely respiratory. To characterize the specifics of her condition, she used the term #LongCovid, thus becoming the first patient to give a name to the illness. Her initial commitment and the subsequent steps that followed evoke an individual empowerment process. How did Elisa Perego transform from a vulnerable patient to an internationally sought-after expert? Selfpower-community investigated…
When did you start writing posts on Twitter/X ?
Elisa Perego: I started writing about Covid on Twitter/X before getting sick. I was very concerned about its early spread, and lack of timely response. As regards Long Covid – ah, but I found an explanation. And the explanation was correct. Covid did not last two–six weeks, like the early reports said, and it wasn’t a respiratory disease only. Of course, I was also very concerned about my health. About my oxygen saturation dropping again and again when I should have been “recovered”. I evoked these symptoms and found that a large number of people were suffering from the same pains
Regarding doctors, what were your feelings?
EP: In early 2020, I was in the early epicenter of Lombardy, Italy. Medical professionals were on the frontline. Many died or experienced Long Covid themselves. I want to express my solidarity to the healthcare professionals who were on the frontline in those early, terrible days. I do believe, however, that by now, in 2024, healthcare should be much better equipped to deal with Long Covid. Too many remain with no adequate medical support. In 2020, there was also poor acknowledgement of how dangerous and “long” Covid could be even in “young” people. Many of us did not receive adequate care because of that, too.
Regarding the healthcare system?
EP: As I mentioned in my previous answer, I was in Lombardy, the early Covid epicenter outside China. The healthcare system basically collapsed. It is not easy to convey this feeling: you understand you most likely have a disease, Covid, you know it can kill you. You also know your healthcare system is at 100% capacity and beyond. No help is coming. Tweeting was very important to me to try to convey how bad the situation was.
What did it bring you to be joined by peers?
EP: It was very important. It showed that what I was experiencing myself, and what I was hearing from my local community, wasn’t an exception. It became crystal clear we were witnessing a massive emergency, which could lead to devastating consequences for global health, if SARS-CoV-2 was not contained. Sadly, hundreds of millions have now been estimated to have experienced Long Covid by several researchers and the World Health Organization.
Can you talk about the collective experience of illness?
EP: This is just my personal experience, it might not apply to others. It felt emotional, empowering and innovative. I saw it a bit through the eyes of the researcher, you see. Being so ill, but also so free to build something new at the extreme frontiers of knowledge. In a completely open access, immersive framework, on Twitter. With new information coming out in real time. With a lot of solidarity among sufferers: the urge to understand, to alert the world, to try to spare others from what was happening to us.
Has being a researcher, familiar with the intricacies of the scientific process, changed anything in your approach to illness?
EP: Yes, it changed . As a researcher, I have the opportunity to understand research by others, and also to produce my own. Medical professionals are, generally, broadly trained to diagnose and treat already known diseases. As a researcher, I can build new knowledge. I have the opportunity to apply emerging biomedical evidence to understanding what’s going on in my body. This affords you to link the science to the lived experience. As I did with Long Covid.
Can you list the actions you have developed?
EP: I can’t provide a complete list of all the things I have done in relation to Long Covid. There are so many! Broadly speaking, I contributed to or co-led efforts that led to the recognition of Long Covid globally: both as a disease entity and as an advocacy/research movement. I attended (virtually) the landmark World Health Organization meeting of August 2020, after which WHO openly recognized Long Covid. I submitted evidence as a patient expert to the National Academies of Sciences, Engineering, and Medicine (NASEM) for the US definition of Long Covid in 2023. I write and peer-review scientific papers. I write, sign and/or revise white papers, open letters, press releases. I am Long Covid Kids Champion for the charity Long Covid Kids. I do a lot of science communication, for example on social media, such as Twitter/X: these are platforms which I consider not only a place to communicate, but also tools to build new knowledge. This is how Long Covid was born. I deliver academic talks, virtually of course, and I engage with the press and policymakers. I have collaborated extensively with researchers, patients and other stakeholders on Covid and Long Covid. A lot, especially in those early frantic months of the pandemic, has been informal: emails, chats, tweets, messages. But it worked to kick start knowledge, awareness, and understanding of Long Covid. Many of us did this as patients. Many such contributions aren’t even acknowledged or known. But now big labs are working on Long Covid. There are official guidelines. Of course, everything I do is greatly impacted by my health. I am still very ill. I can’t do as much as I would like – trying to do my best.
What have these actions brought you in terms of learning, knowledge and skills gains, agency, influence, feeling of regaining control… ?
EP: Agency for sure. I have acquired new skills, for example in terms of approaching policy and advocacy on a global scale. I wasn’t dealing with the press or high-profile policymakers before Long Covid! I have become much more proficient in research fields such as infectious diseases, biomedicine, and epidemiology. They were linked to my most recent research before the pandemic, but I have a stronger expertise now.
What path do you think you have opened up?
EP: The experience of Long Covid showed that patients can provide ground-breaking contributions to knowledge. They can change how knowledge is built, and develop innovative solutions to devastating challenges, such as the Covid pandemic – one of the greatest health disasters in recent history. Patients can change how diseases are named, defined, recognized.
Being so confronted with the dysfunctions of the healthcare system prompt you to have a different understanding of its organization?
EP: Yes, I think we truly need healthcare systems to be better equipped to dealing with chronic diseases. And we need healthcare systems that are ready to acknowledge patients as partners. I am chronically ill from before Long Covid, too. I know the challenges too well.
How do you continue your commitment?
EP: I continue to write scientific literature and advocate for the rights of people living with Long Covid and people with disabilities/disabled people. I continue to advocate for full recognition of Long Covid and containment of SARS-CoV-2. I am still doing a lot of science communication and research, including research-related activities (peer review, etc.). It’s not a 9 to 5 job. I am currently too sick to have a job. It’s a bit hectic.
And what advice would you give in case of a new pandemic?
EP: This advice is for policymakers and public health. Please act as early as possible. Go for containment of the pathogen, virus or otherwise, as hard as possible. Go for eradication and elimination if possible. Be transparent with data. Acknowledge immediately how the pathogen transmits, and act appropriately. For example, if a virus is airborne, such as SARS-CoV-2, take airborne precautions. Be fully aware that death is not the only clinical outcome that matters: the long-term health effects of infection matter too, like with Long Covid. Put human life and global health above short-term economic and political gains.
With hindsight, what do you consider to be the current priority for healthcare systems?
EP: We need timely, high-quality, free healthcare for all, including in countries with a poor tradition of public healthcare, or where public healthcare is now failing. We are facing a great challenge in this regard, because healthcare services are under duress in view of ongoing SARS-CoV-2 spread and austerity policies. Second, we need a much better approach to chronic diseases, especially those which are poorly addressed in current medical practice. Third, Long Covid is a global emergency. Healthcare systems need to be strengthened substantially for dealing with this growing influx of patients.
How would you define patient empowerment?
EP:You have the right to name a disease. You have the right to define a disease. You have the right to make policy. You have the right to contribute to clinical case definitions. You have the right to contribute to guidelines. You have the right to do patient-led research, if you want to. You have the right to ask policymakers to make this possible. You have the right to treatment. You have the right to say no, if something is making you worse. You have the right to be an equal partner in your care. You have the right to dignity. You have the right to go to the doctor and feel free to discuss your concerns safely. You have the right to Google your disease, and read the scientific literature, and talk about it with your provider, openly. I know a lot of this is not a reality for many patients. It’s an ongoing fight. Epistemic injustice is rife in medicine. There are constraints due to time and resources. But there are also constraints caused by ableism, and by the way in which medical professionals are trained, by the lack of agency patients are sometimes afforded. We need capillary change.
Analysis
Elisa Perego followed all the stages of individual empowerment: recognizing dysfunctions, sharing her experience with other patients, using a social network as a platform for co-creating new knowledge, asserting her identity, regaining control over the illness, gaining autonomy, expertise, skills, and societal influence to defend the interests of patients. Her uniqueness lies in positioning herself in the research field by adopting a scientific stance to analyze her illness and its medical and social treatment.
Her profession as an archaeologist and her experience with the disease led her to track the evolution of human societies’ health : “Health is not a given but is shaped by inequalities and political choices.”(3 Starting from this observation, she questions the health option that acknowledges the existence of “endemic Covid,” a strategy she views as less demanding and ultimately more discriminatory than the “Zero Covid” goal, which aims for its total eradication as was the case with smallpox.
By following the usual steps of any research process—observation, description, hypothesis development, experience confrontation, analysis, and interpretation—she created her own study. Her work was conducted in extreme urgency. New information was posted in real time. Community members explored the boundaries of knowledge in an immersive, supportive, and entirely free-access framework. All shared the same need to understand and alert the world to spare others from what they were experiencing.
Elisa Perego relied on her research expertise. She decoded scientific publications and highlighted new contributions from her own analyses. She learned to interpret her symptoms in light of the latest biomedical data.
Thus, a patient was able to construct scientific knowledge without intermediation. She contributed to the global recognition of long Covid as a pathology. Her analysis of patients’ experiences led her to question the orientations of certain health policies. Elisa Perego continues her advocacy by promoting the integration of patients into the conceptualization, study, and treatment of COVID-19
Redaction : Elisa Perrego and Marie-Georges Fayn
________________________
(1) Individual or psychological empowerment: an initiatory process that transforms a vulnerable individual determined not to endure a situation anymore, into a resilient person. This person becomes aware of their weaknesses but is able to overcome them through acquiring knowledge and adapting behaviors..
Psychological empowerment is measured by several criteria
[3] World Socialist Web Site https://www.wsws.org/fr/articles/2022/10/13/inte-o13.html





En postant un commentaire sur www.selfpower-community, vous acceptez les règles de l’espace réaction et reconnaissez à www.selfpower-community la capacité de ne pas publier certaines contributions sans avoir à motiver cette décision.
prendre connaissance des règles