Health empowerment scales (1997-2019)
69- 01/11/2023 As empowerment is nowadays a central concept in healthcare system, the examination of four measurement scales aims to provide a modest contribution to understanding the evolution of patients’ autonomy and emancipation over the past two decades. This work was first presented at the 8th European Conference on Health Communication (nov 2023, Klagenfurt, Austria)
The analysis reveals that empowerment is intricately tied to our individual perceptions of illness and our unique understanding of power dynamics. It depends also on context, on the ability of professionals to integrate the patient’s perspective and on the information and communication technologies allowing the multiplication of horizontal exchanges. Understanding empowerment also depends on effective measurement
This work is an invitation to step back and reflect on the meaning of empowerment for patients faced with the vulnerability of the human condition.
– How will they cope with adversity?
– Take control of their destiny?
– Learn to manage their health individually and collectively, so as to live as equals?
Each research project brings its own answers and enriches general knowledge.
Empowerment is recognized both as a state andas a result of a process or as a process in itself.
At the individual level, patient empowerment encompasses a range of feelings such as
– self-esteem,
– efficacy,
– self-control,
– awareness,
– determination
– and autonomy
Patient empowerment and our relationship to illness are closely linked.
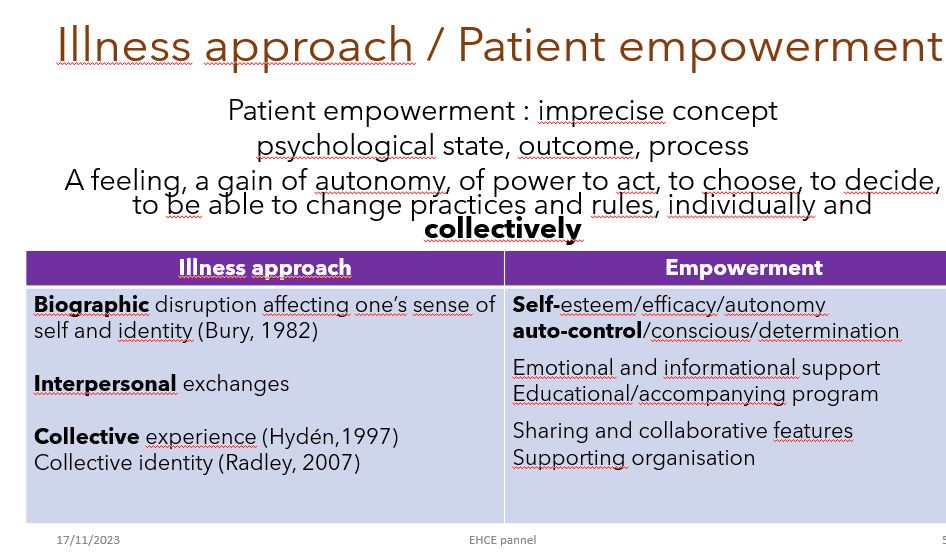
When entering sickness, individuals are confronted with the ordeal of fragility and a biographical disruption. The challenge of empowerment is to reappropriate a positive identity partially eroded by this experience.
However, today’s patients are no longer isolated and fragile individuals. Patients with long-term conditions are encouraged to become involved throughout their care journey, codecider of their treatment taking into account their own values and life goals.
This calls for open-mindedness and teamwork skills on the part of professionals, involving patients in the care process, sharing and managing their medical records with them. It also involves therapeutic education sessions in which patients actively participate alongside care providers. With the emergence of patient associations, forums and networks, illness has become a collective experience to decipher together. Patients become engaged participants, in constant interaction with organized, influential and well-informed online communities. Thousands of patient associations are demonstrating solidarity and innovation, improving daily life by helping each other overcoming obstacles and combating inequality and stigmatization (Rappaport, 1987; Laverack, 2006).
Thanks to better and more accessible digital platforms, these online communities are playing an essential and growing role in the individual and collective patients empowerment ;
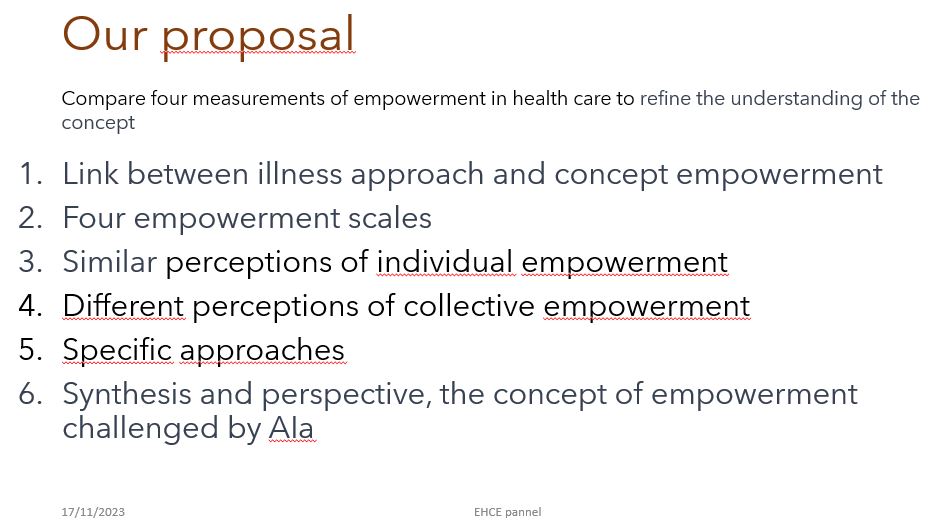
Four mesurement scales
Experienced patients – called patient experts or patient resources – are invited by institutions to co-construct the healthcare system (Wallerstein, 1992, 2002, 2006). The four measurement scales selected illustrate four different approaches four complementary visions of empowerment that help to appreciate its multidimensional nature.
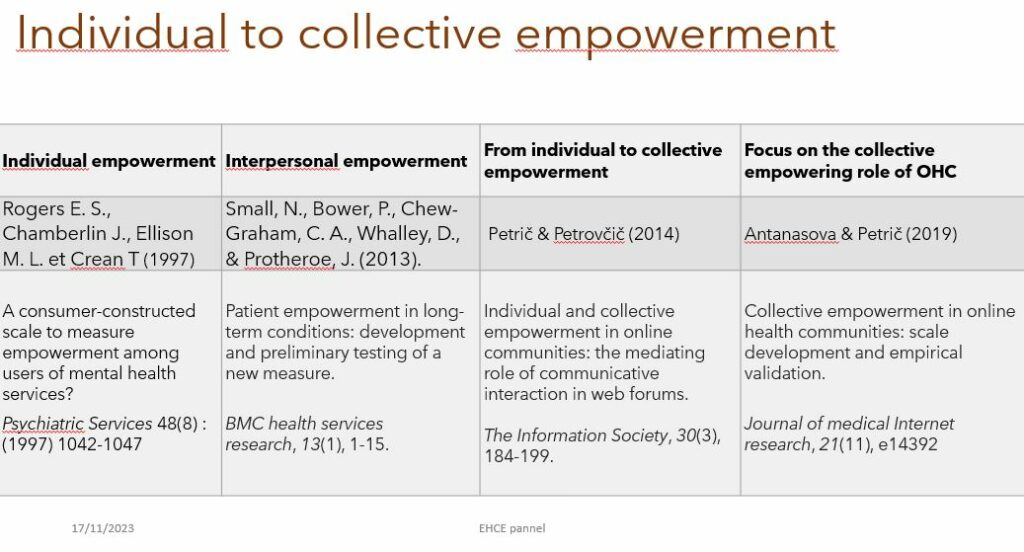
First : an individual, patient-centered approach with Rogers and al (1997) who published a consumer-constructed scale to measure empowerment among users of mental health services.
Second : an internal process and external relationships forged with care professionals and other patients, by Small and al (2013)
Third Conditions of congruency between individual and collective empowerment on online communities by Petrič and Petrovčič (2014).
Forth Online communities as collaborative resources booster by Atanasova, S., & Petric, G. (2019). So each team has its own conception and definition of empowerment
Four definition of empowerment
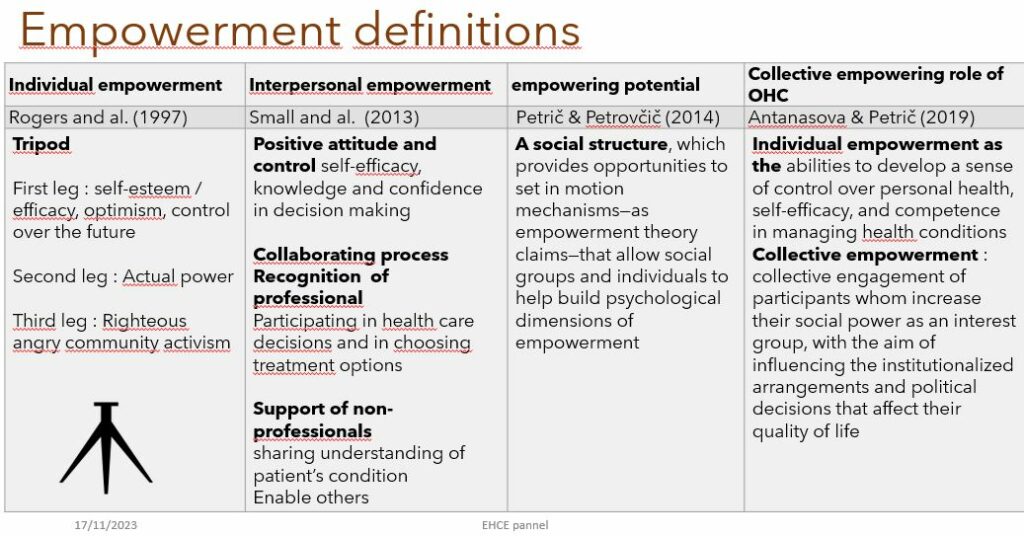
For Rogers and al. (1997) empowerment is like a Tripod supported by
First leg : self-esteem / efficacy, optimism, control over the future
Second leg : Actual power
Third leg : Righteous angry and community activism
For Small et al. (2013) empowerment leads to a positive attitude, improving patient’s
feelings of control,
self-efficacy,
coping abilities,
and ability to achieve change over their condition through an enabling process with the health care professional and mutual peer sharing of resources and information.
They recognize a process of pooling and collaboration in interpersonal empowerment.
Petric and Petrovic (2014) approach empowerment through the empowering potential of the social structure of an online community, which enables social groups and individuals to contribute to the construction of the psychological dimensions of empowerment. The dimensions includes
sense of adequacy of one’s task and one’s values,
ability to fulfill one’s mission (competence),
autonomy and control over one’s activities (self-determination),
and influence on a wider environment, both institutional and social (impact) (Hur 2006).
These psychological resources not only help individuals to improve their social position but also help the group itself to take control of resources, gain recognition by deciders and acquire power in society.
Antanasova & Petrič (2019) define individual empowerment as the abilities to develop a sense of control over personal health,
self-efficacy,and competence in managing health conditions.
collective empowerment refers to the collective engagement of participants who increase their social power as an interest group with the aim of influencing the institutionalized arrangements and policy decisions that affect their life.
In this sense, Online Health Communities (OHCs) facilitate discussions on topics related to political issues such as
– access to or provision of health care services,
– health inequality,
– disease prevention,
– patient advocacy,
– health care reform,
– patients’ rights,
and power relations in healthcare.
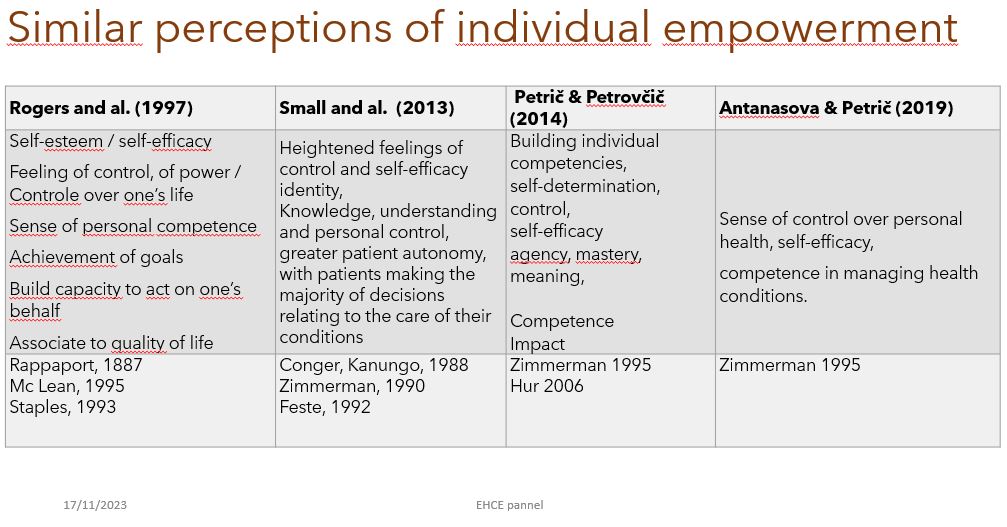
Important to note that there is a near-consensus on the definition of individual empowerment based on Zimmerman’s reference(1990-1995) who identified its main criteria:
contrôle,
self determination,
self efficacy building, capacities and competencies.
But there is no consensus on collective empowerment
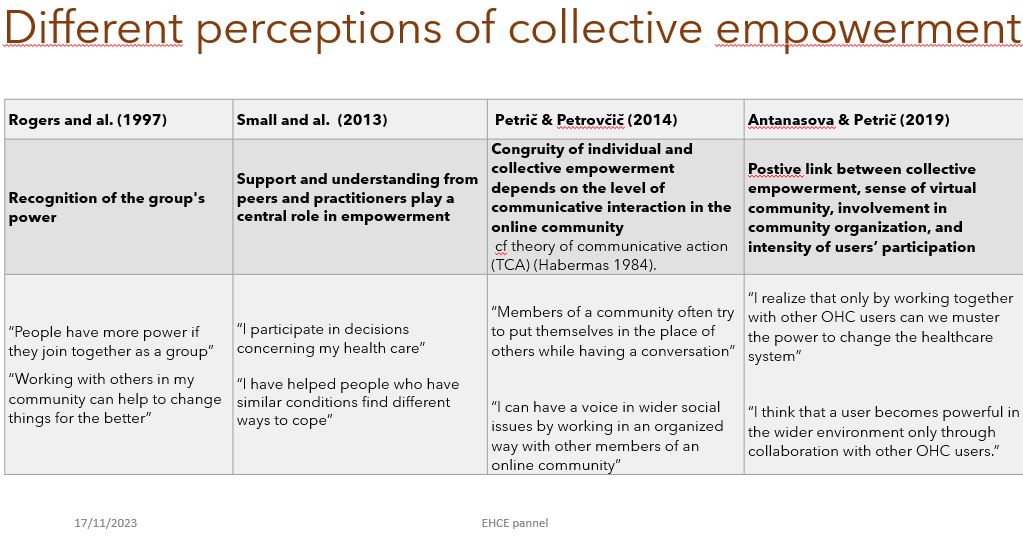
Rogers et al. (1997) point out the patients capacity to turn anger into action. They knowledge that the group shifts the balance of power which becomes more favorable to patients,without fully apprehending its scope of intervention or internal organizational modalities.
Small and al. (2013) incorporate the increasing role of non-professionals and their growing presence in supporting and imparting knowledge to patients. They highlight the importance of the relational dimension in empowerment, relations with two kinds of public, health care professional and peers
Petric and Petrovic (2014) focus on how a group of people gains psychological capacities to change its disadvantaged social position (Hur 2006), with an emphasis on the level of communicative interaction, a concept derived from Habermas’s theory of communicative action (Habermas 1984). They recognize that collective action based on reciprocal support and coordination of community members is needed for the community to gain influence and, consequently, produce sociopolitical changes.
When the sense of community is accompanied by communicative social interactions, members not only develop feelings of collective agency but also attain greater self-esteem and self-confidence (Tanis, 2008). They distinguish authentic communicative action aimed at increasing knowledge and skills and strategic action aimed at maximizing impact, close to manipulation.
It’s only through the strengthening of interpersonal relationships with other community members that individuals can have an impact on wider social circumstances.
Antanasova and Petric (2019) balance this position. They note a positive link between collective empowerment, sense of virtual community, involvement in community organization, and the intensity of users’ participation.
However, there is a weak correlation between involvement in a community’s activities and understanding the wider sociopolitical contexts of health issues and how to collectively engage to influence such contexts.
The authors suggest that integrating various subcommunities can enable users to better master health-related knowledge, choices and issues.
They emphasize the importance of two complementary factors: collective resources such as actions, strategies or assets acquired through collaborative efforts, and the ability to mobilize them through collective awareness, commitment and action, to jointly influence the wider social structure.
In conclusion, each study, in its own way, advances our understanding of empowerment.
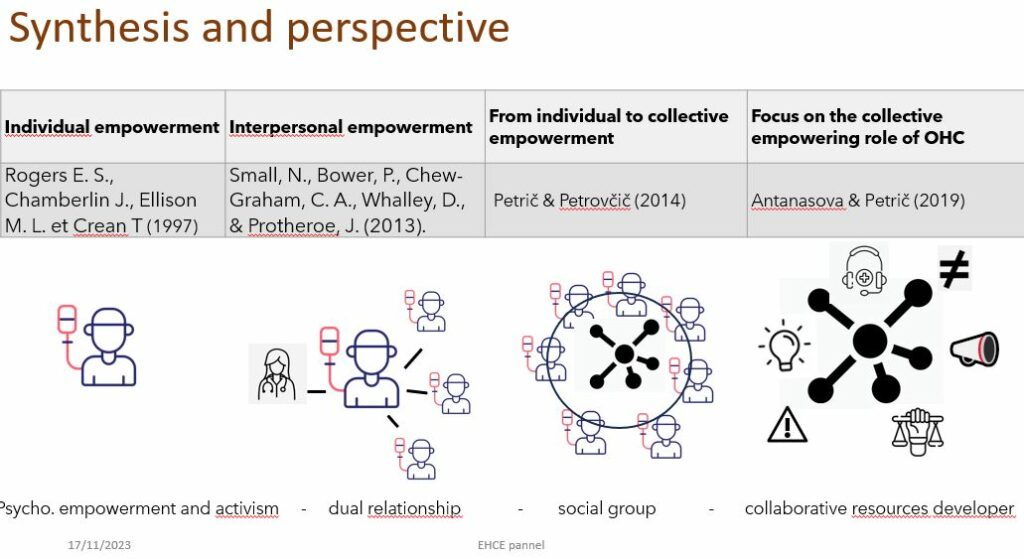
While there is a consensus regarding the criteria for individual empowerment – control, self-efficacy, gaining knowledge, and mastery of one’s condition, the concept of collective empowerment is more problematic for several reasons :
– lack of standardized definition,
– influence of contextual factors,
– social nets and organizational governance,
– complexity of group dynamics which may have different perspectives, goals and power structures.
In addition, the interconnection and the digital functionalities, as well as the activities of sub-groups add another level of complexity.
Despite these challenges, researchers’ work identifies strong trends in collective empowerment recognizing the unparalleled opportunities offered by networs enabling, under certain conditions, the creation of collective intelligence and mobilization. The study highlights the increasing role of non-professionals in supporting and transmitting knowledge to patients. This rise in patient empowerment leads to a redefinition of the roles and relationships between patients and healthcare professionals.
Patients’ connections with peers facilitate the sharing of narratives, the development of a critical understanding of health issues, a marked resistance affirming the patient voice through the appropriation of health discourse and the claim of expertise. Through their communities Patient engage collective actions to influence and tranform the sociopolitical environment.
Given the patients communities developments in the healthcare sector, understanding how communities can collaborate to create positive change is essential.
This work as a milestone in the constantly evolving definition of empowerment. The next step will certainly take into account the development of artificial intelligence.
In terms of empowerment there will be a before and after AI
The AI tools grow in number and in complexity facilitating self health-control and monitoring. This phenomenon* will lead to a shift with our relationship with illness, with the traditional healthcare offer, with the professional practices and consequently, with our very conception of empowerment.
| Marie-Georges FAYN Associate Researcher, VALLOREM laboratory Tours (France) |
Samy MANSOURI Associate Professor, IAE Orléans University School of Management VALLOREM laboratory, Orleans (France) |
Bibliography
- Bury, M. (1982). Chronic illness as biographical disruption. Sociology of Health and Illness, 4(2), 167e18
- Hydén, L. C. (1997). Illness and narrative. Sociology of health & illness, 19(1), 48-69.
- Rappaport, J. Term of empowerment 1987
- Stapples, L. Consumer empowerment 1993
- Mc Lean, A. Empowerment and the psychiatric
- Zimmerman MA. Psychological empowerment: issues and illustrations. Am J Community Psychol 1995 Oct;23(5):581-599.
- Petrovcic A, Petric G. Factors of collective psychological empowerment of active users in the online health community med.over.net. Slovenian J Public Heal 2014;53(2):133-143
- Radley, A., & Bell, S. E. (2007). Artworks, collective experience and claims for social justice: The case of women living with breast cancer. Sociology of health & illness, 29(3), 366-390.